To view this on my website, search for other blogs, and sign up for future posts, please click here.
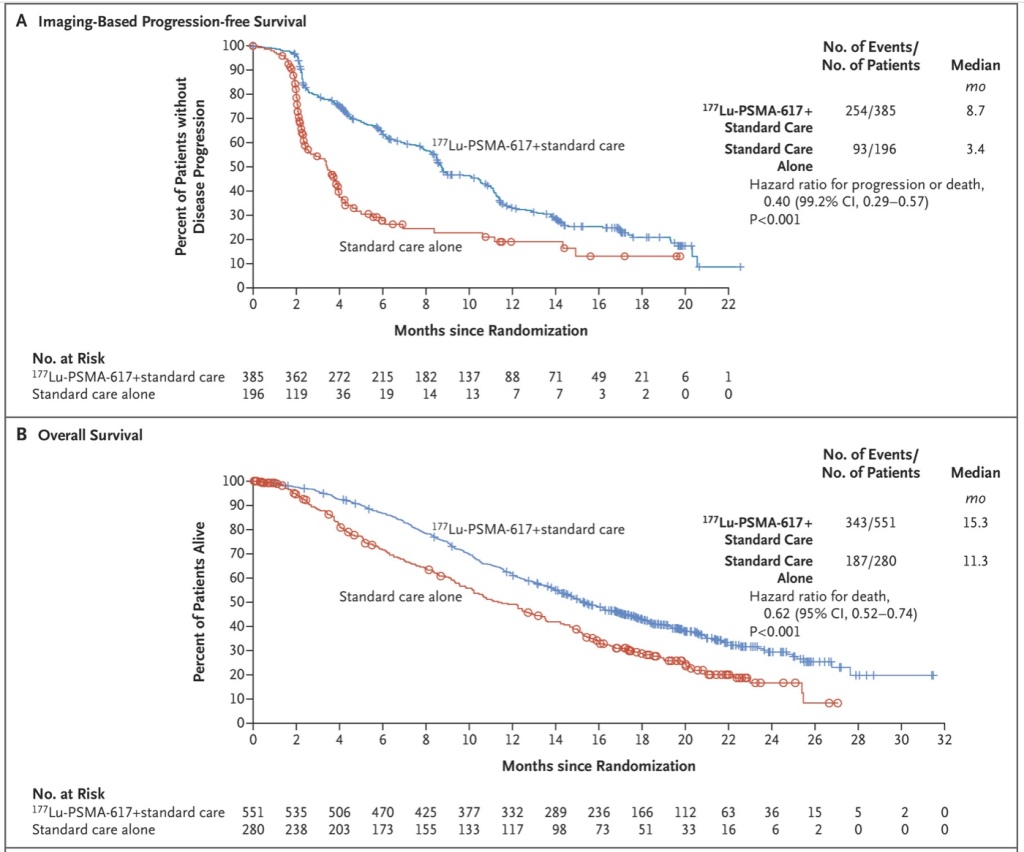
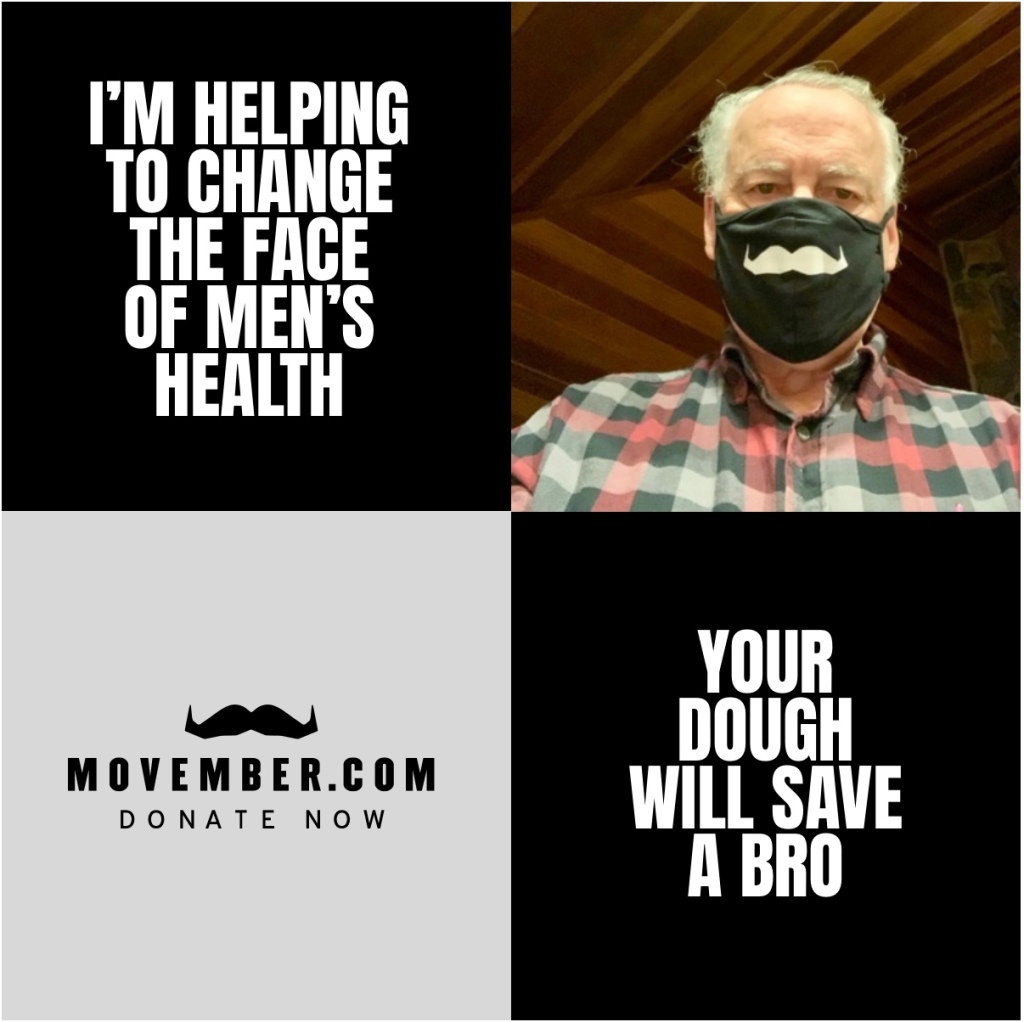
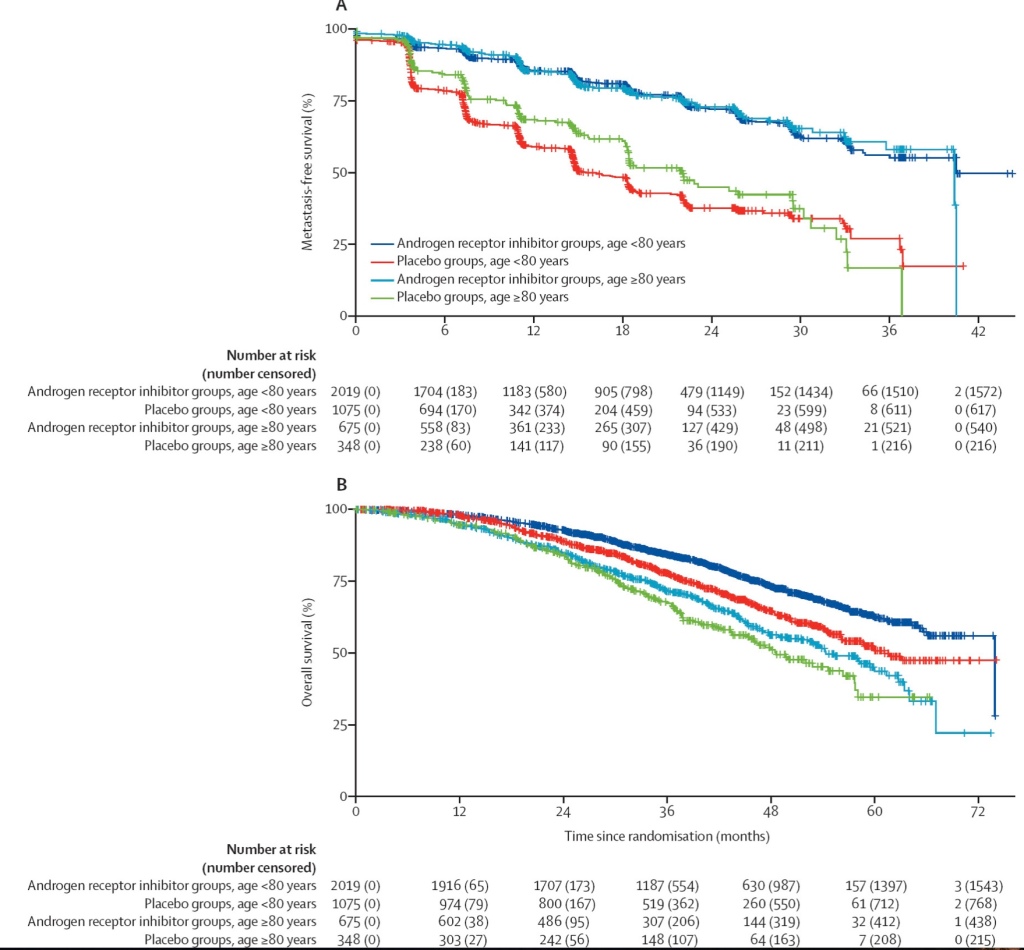
I want to wish all of you a very Merry Christmas, happy holiday (whichever ones you celebrate or just celebrated) and a safe and vaccinated New Year. And most of all, THANK YOU to the many folks who contributed to my annual Movember Moustache. We again blew the top off my goal, and it makes me abundantly happy to join you in supporting the research into prostate cancer survival and cure.
Second, I urge you to hang in there, wear your masks, and limit the Christmas interactions. We only have a couple of months to go before we are vaccinated if you are in my age bracket, so stay the course!
Finally, I will share the thoughts of my Department of Medicine Chairman, David Schwartz who has put as fine a summary on where we have been and where we need to go as I have seen. I hope you will find it encouraging:
“A number of months ago, I wrote that ‘Science will lead our way out of this crisis. Basic modeling and infectious disease epidemiology has helped us understand what’s coming, the science of social distancing, clinical trials have identified remdesivir as a promising agent, novel serologic assays will identify the extent of disease in our communities, and vaccine development will provide the cure. All of this takes investment, and now is not the time to back away from our scientists or our scientific infrastructure. In fact, now’s the time to double down. We still have to get through this crisis but rest assured there will be human health challenges in the future, and we need to be ready.’
Now with the demonstrated importance of social distancing, the improved care of patients with Covid, and the FDA emergency use approvals of the Pfizer and Moderna vaccines, it’s time that we recognize and celebrate the truly remarkable advances in our fight against Covid that have been made since the initial transmission of SARS-CoV-2 in the Huanan Seafood Wholesale Market only one year ago.
· Social distancing: The past few weeks have demonstrated the profound effect that social distancing has had on the transmission of the virus. The story of the coronavirus in America is a compartmentalized one, with different places experiencing different spikes for different reasons at different times. Fortunately, over the past week in Colorado, there’s been an average of about 3,100 cases per day, a decrease of 28% from the average 2 weeks earlier. This decrease in cases per day in Colorado is reflected in the census data in our hospitals, and the state-wide hospitalization data with both peaking and slowly going down since the beginning of December. In contrast, over the past week in the entire U.S., there’s been an average of about 220,000 new cases per day, an increase of 19% from the average 2 weeks earlier. Continue to wear a mask, practice social distancing, and don’t travel over the holidays.
· Clinical trials: Over the past year, well-conducted clinical trials (by many of our investigators) have identified what works and what doesn’t. Our improved ability to take care of patients with SARS-CoV-2 infection is reflected in the decreased percent of patients requiring ICU care (55% last spring – 40% now) and a decrease in the number of patients in the ICU requiring intubation (90% last spring – 67% now). Moreover, the survival and re-admission rates continue to improve among our Covid patients.
· Vaccines: One year ago, very few people would have predicted that we would be embarking on a vaccination program with two extremely effective vaccines with minimal side effects. This was not a miracle. The development of these vaccines were enabled by many scientific accomplishments (bat virology, DNA sequencing, computational biology, and basic science of RNA, proteins and lymphocyte biology to name a few) that have been supported by the federal government, industry, academia, and public-private partnerships. Investments in science are essential to our future.
I think there are other take home-messages that will continue to strengthen the scientific programs on our campus:
· Team science and scientific partnerships are critical to combining clinical insights with cutting–edge research. Collaborations and social networking will improve the efficiency of research. We need to foster these interactions.
· Public-private partnerships (like the one between the NIH and Moderna) can lead to powerful advances and need to be nurtured.
· Our nation has to place a higher value on science. Part of this involves public education and we’ve got some real opportunities with our patients. However, we should also do everything possible to help Congress recognize the sad lessons learned from the ways science has been pushed aside during the pandemic, and strongly advocate to substantially increase the federal research budget.”
To all of you who subscribe to this blog, I thank you for your interest, ideas for topics, and your support for the physicians, nurses, staffs and researchers who have made it possible for all of us to live longer and healthier lives than any generation in history. It has been an incredible journey for most of us and in spite of the 2020 “downer” we have much to be thankful for. Keep exercising and my best wishes for the New Year!