To view this on my blog, sign up for future posts, and search for other posts regarding prostate cancer issues, please click on this link.
We made it around the sun another time, and in spite of Covid 19, are still here to thank you for your interest in this blog and most especially for your support of prostate cancer research via my annual efforts to grow a moustache and help Movember raise funds for prostate cancer research. A heartfelt thankyou!!
With all of the “Ten best” and “top songs” lists that appear this time of the year, I thought I would expand a bit on PSMA as a real game-changer that is coming on strong to change our management of prostate cancer. So what is Prostate Specific Membrane Antigen?? Well, first of all, I think you know what an antigen is, or if not, here’s a timely clue: Spike protein. When you received your vaccination with Moderna, Pfizer or J&J vaccine, you were exposed for the first time to a foreign protein that the SARS CoV2 virus (COVID-19 disease causing) uses for entering the cells that line your airways. Your body responded to this antigen (foreign protein) by developing antibodies – the levels (titers) of which prevented you from getting COVID, or at least prevented you from getting very sick. Antibodies are very specific proteins made by the B-cells of your immune system that bind to foreign antigens and are the first line of defense against invaders.
Now, if you inject a mouse with human prostate cells, the mouse will recognize all sorts of the proteins as “foreign” and make antibodies against them. In such an experiment, Wright and colleagues in the early 1990’s found that one such antibody could be useful in detecting prostate cancer. It turned out that the antibody was detecting a protein expressed on prostate cells, but also tumor blood vessels and the salivary gland that became known as PSMA. Unlike PSA, this protein is bound to the membrane of the cancer cells and doesn’t circulate in the blood stream. PSMA is actually an enzyme involved in the normal absorption of folate (a vitamin) from the intestine, but for unclear reasons, it is dramatically over expressed by prostate cancer cells. Over the next 25 years, numerous researchers worked on tagging radioactive isotopes to antibodies that would bind to PSMA and therefore could be used to detect prostate cancer or if the radioisotope was powerful enough, kill prostate cancer cells. One of the challenges, however, in using radio labeled antibodies is their size, resulting in a lot of non-specific “sticking” in the liver, spleen and elsewhere. A better approach evolved by finding small molecules that would stick to the PSMA enzyme activity site as illustrated in this figure:

As a result of this research, it became possible to develop highly sensitive PET scans that can detect much smaller metastases of prostate cancer than any previous bone or CT scans were able to do. Gallium and Fluorine isotopes hooked to the peptide (617) are rapidly becoming available in PET scan centers across the United States (and have been available for the past 3-5 years in Europe, Australia and elsewhere) and will likely become approved as the new standard for staging newly diagnosed and PSA recurrent metastatic prostate cancer. Moreover, the isotope Lu177, that emits strong beta radiation (electrons) can be attached to peptide 617 and kill cells that express PSMA.
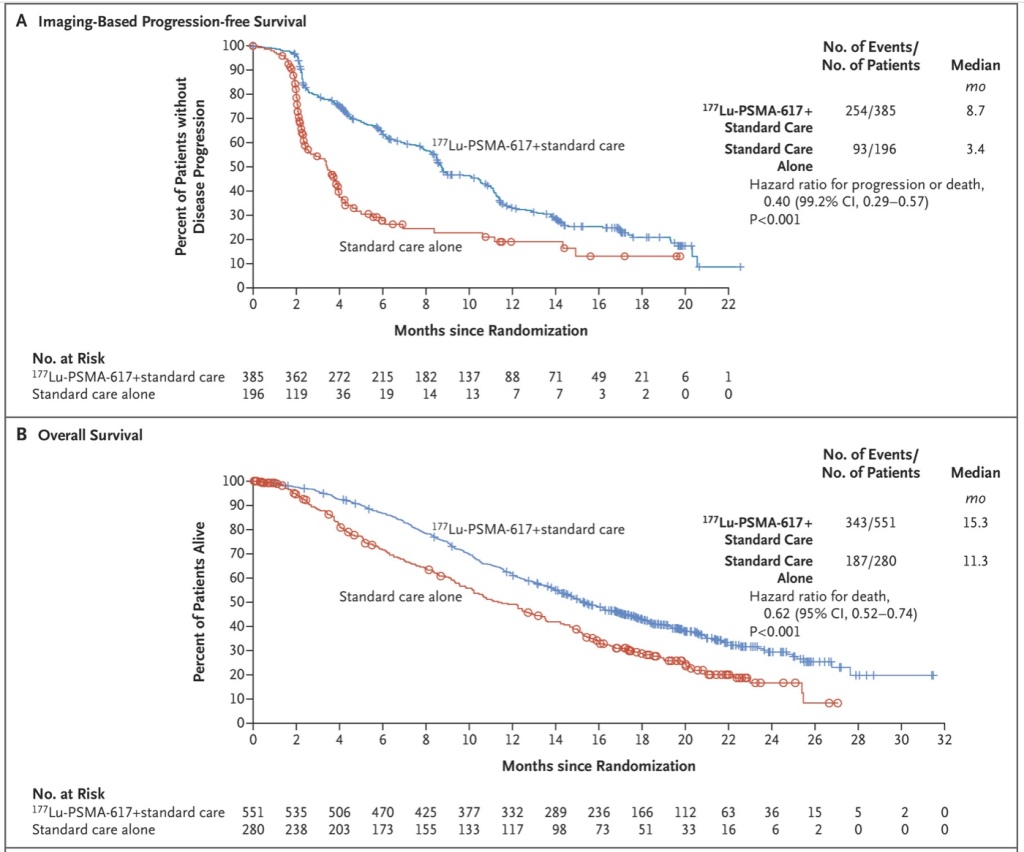
In the VISION trial, published this year in NEJM, the use of Lu177 PSMA to treat advanced prostate cancer patients who had progressive disease after previous treatment with a second generation hormone agent (such as Zytiga or Xtandi) plus chemotherapy with a taxane (Taxotere or Jevtana) were scanned with Gallium labeled PSMA then treated with Lu177 PSMA. The treated men were compared to alternative “standard of care” which might have included other forms of chemotherapy for example. The results were extraordinary as shown in these curves.
So for this year, I’m nominating PSMA as the molecule of the year. PSMA PET scans will likely be the only scans needed to follow prostate cancer metastases, and are already being used in newly diagnosed patients with high risk disease to make sure we don’t miss something. Further, if there are only a few metastases, we can treat these at the same time we treat the prostate with hopes that some of the patients with metastatic disease can still be cured. And ongoing research is underway to evaluate the use of Lu177 PSMA in earlier patients without resistant disease. Great progress and I leave you with fond wishes to you and your family for a healthy (VACCINATED) 2022!




Superb summary! I agree with your nomination of PSMA as the molecule of the year. Now, when can we expect the PET scans with PSMA in Colorado? How long will it take for this information to filter out to the practice community?
As always you simplify complex science so we can understand it.
Happy Holidays to you and your family.
Bob
Yes, completely agree! Very sad that it’s not available now for those in need of it.
HI Bob,
scans are just now becoming available in CO but therapy seems like it is still a ways off. See other comment for details.
PSMA Pet now pretty widely available. Check with Rocky Mtn Cancer Centers or CU Anschutz.
Thank you for invaluable information should the need arise. Very well explained for non medical people such as I.
I heard from my urologic oncologist at UC Health that, perhaps, Rocky Mountain Cancer Centers may have, or soon have, the PSMA scan. Anyone know about this?
As I understand it, scans are now available using the F-18 isotope (Pylarify) at RMC – not sure which location. That PSMA product is being made in Arizona I think, then shipped to Denver with enough to do 4 patients on the same day. It will be a while before the availability is similar to the F-18 deoxyglucose which is the “standard” reagent used for “pet scans” for cancer (and doesn’t work as well for most prostate cancers. I believe CU nuclear medicine is gearing up to make the PSMA Gallium-68 reagent which requires a cyclotron and has a very short half life so has to be made “on site” and then immediately injected. There seems to be little difference in sensitivity/specificity between the two. The remaining challenges include reimbursement and which patients qualify for ordering the scans (currently only those with rising psa after definitive therapy I believe). I suspect that eventually all high risk newly diagnosed patients will get a PSMA scan and it will become the standard of care for following prostate cancer as much as the PSA is used.
“… patients qualify for ordering the scans (currently only those with rising psa after definitive therapy I believe)”
Yes, that is what my doctor mentioned to me. I am successfully on Orgovyx right now so the PSMA scan is sometime in my future…hopefully a long time.
Thank you for your informative reply!